Frozen Shoulder
The shoulder joint is a ball and socket joint. Most shoulder movement occurs where the ball at the top of your arm bone (humerus) fits into the socket (glenoid) which is part of the shoulder blade (scapula). The rotator cuff muscles are a group of muscles whose tendons form a ‘hood’ over the head of the arm bone (humerus). These muscles control the stability of the joint and the finer movements. The lining or sack (capsule) is extremely loose thus allowing much movement between the ball and socket joint.
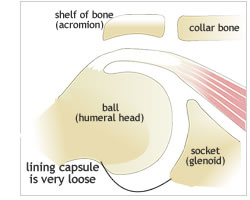 In frozen shoulder the lining (capsule) of the shoulder becomes scarred, thickened and very much contracted resulting in the joint becoming very stiff. In addition scar tissue forms between the head of the arm bone (humerus) and rotator cuff tendons thus further limiting the movement. This loss of movement is accompanied by marked pain. The reason why this condition occurs, the fact that it is peculiar to the shoulder and the fact that itrecovers of it own accord remains somewhat of an enigma.
In frozen shoulder the lining (capsule) of the shoulder becomes scarred, thickened and very much contracted resulting in the joint becoming very stiff. In addition scar tissue forms between the head of the arm bone (humerus) and rotator cuff tendons thus further limiting the movement. This loss of movement is accompanied by marked pain. The reason why this condition occurs, the fact that it is peculiar to the shoulder and the fact that itrecovers of it own accord remains somewhat of an enigma.
Would you like to see a doctor?
Learn more
Cause
The exact cause of a frozen shoulder is not known but it may begin after a minor injury. It is more common in certain conditions:
1. Diabetes – it is very common in diabetics and tends to have a worse prognosis in these patients.
2. Underactice thyroid
3. Ischaemic Heart Disease
4. Previous neck problems
5. Nerve conditions
6. After operations: eg: breast surgery, cardiac surgery and shoulder operations
7. Idiopathic – In most patients, it occurs without any predisposing factor.
Diagnosis
It is more common in women and occurs in the age group from 40 to 60.
The pain of frozen shoulder can be from a minor irritation to severe pain. The pain is often unrelenting and is usually worse at night. It is often felt over the mid part of the arm and not the shoulder itself. Patient usually tolerate the pain during the day but if they do a sudden unexpected movement, the pain is often nauseating but lasts for a couple of minutes only. The night pain is often distressing and patients suffer from chronic fatigue which can result in an element of depression.
One of the classic features of frozen shoulder is severe nauseating pain with sudden movements or jerking of the arm, this makes the patient stop and usually last for seconds or minutes. This is called the ‘JERK PAIN’.
In the initial phase, pain is the main symptom but the patient’s range of movement is normal. It this initial phase it is more difficult to make the diagnosis as it may present just like tendonitis of the rotator cuff. The movement slowly gets worse and the first thing that the patient notices that they cannot do is get their hand behind their back i.e. to do up their bra.
Course of Natural History of Frozen Shoulder
The disease goes through 3 characteristic stages:
Phase 1 – PAINFUL OR FREEZING PHASE
An otherwise healthy person develops slow onset of a generalised aching in the shoulder. Pain is constant, nagging, worse at night and is aggravated by moving the shoulder. Often the only thing that will prevent the pain is keeping the arm still close to their side. A common precipitating event is when the arm is extended and internally rotated ie: reaching into the back seat of the car from the front to lift something. This event is often forgotten. Pain killers and anti-inflammatory tablets do not help the pain much. The length of this phase varies from 4 to 9 months.
Phase 2 – ADHESIVE, FROZEN OR STIFFENING PHASE
The pain settles down and the shoulder remains very stiff. There may be a different pain now which is a muscular pain over the shoulder blade. Because of the stiff joint extra stress is put on the shoulder blade and its muscles thus causing pain. This pain is not as severe as the pain in phase 1. This phase generally lasts from 4 to 12 months.
Phase 3 – RESOLUTION OR THAWING PHASE
During this phase, the pain eases and the stiffness slowly improves. In some patients the improvement is very dramatic ie: patient says ‘it got better overnight‘. This phase may last from 5 to 26 months.
Treatment
TREATMENT OPTIONS
Carter Rowe an eminent American Shoulder Surgeon stated about Frozen Shoulder:
‘We have all had to claim that the idiopathic frozen shoulder is a self-limited condition and that the majority of patients become pain-free with a full range of motion within a year to 18 months. Our problem has been: How can we shorten the painful period effectively?’.
This will depend on the stage and tailored to the patient’s individual needs.
1. Pain-killers
The effectiveness of these is variable and usually very strong ones are necessary.Initially mild ones will be tried. These will often only be needed at night.
2. Anti-inflammatories
Usually do not help. Celebrex has been advocated in the early phase.
3. Injections into the shoulder
The effect of these is variable, they may only give temporary relief of the pain but insome cases they may hasten the end of the first phase.
4. TENS – Transcutaneous Electrical Neural Stimulation
This can be very effective in some patients and is administered by a physiotherapist.
5. Sleep
Pain at night and the inability to sleep is a major problem.
It is more comfortable to sleep in a recliner or propped up in bed. Laying the arm on pillows is helpful. A heating pad can be beneficial.
The use of Amitriptylline (normally an antidepressant) has been shown to be very effective in helping the patient sleep.
6. Physiotherapy
Any attempts to stretch the joint to improve movement will just exacerbate the pain.
Local therapy is however very helpful and massage of the periscapular muscles.
7. Exercises
It is important to maintain the movement that one has but not to stretch past the limit as this will just exacerbate the pain.
8. Manipulation
Its use is controversial. It may shorten the frozen phase of the syndrome.
The timing of manipulation is important: if done too early ie: in the freezing phase, it can make the pain worse and lengthen the duration of the freezing phase.
9. Arthroscopy and release
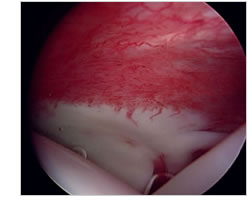
Increased vasculature in the capsule / lining of the joint
Looking in the shoulder with an arthroscope can better define the stage and then a release can be done. The results of release with the arthroscope and results of manipulation have been shown to be the same.
As with the manipulation, the timing of this is very important. Some surgeons advocate this in all patients but there is no evidence to show that it changes the natural history of the condition.
An arthroscopy and release is done as a last resort in a patient in which no other forms of treatment have been able to control the pain.
Increases vessels seen in the joint capsule or lining in a frozen shoulder.
Different treatments or medication will work for different patients, thus patients must find what works for them and take that treatment till the condition recovers of its own accord.
NO TREATMENT HAS BEEN SHOWN TO EFFECTIVELY ALTER THE NATURAL HISTORY OF FROZEN SHOULDER. IT IS THUS THAT SUPPORTIVE TREATMENT ONLY IS NOW ADVISED.
Surgery procedure
Shoulder Arthroscopy
Most surgical procedures of the shoulder are now performed with arthroscopy. This involves the inserting of a telescope (fibre optic) through a thin tube in small incisions around the shoulder. The incisions are between 0,5 to 1,0 cm in size and between 2 and 6 incisions are used depending what operation is done. A single stitch or suture is used to close the incisions after the operation.
This is less invasive but the operation inside is the same as those done with an open operation and thus recovery may still take months depending on the procedure performed.
ARTHROSCOPIC PUMP
To facilitate the arthroscopic (keyhole) surgery, fluid is pumped into the shoulder. This opens the spaces in the shoulder and prevents bleeding. During the procedure some fluid leaks into the tissues around the shoulder which can become very swollen. This fluid is absorbed over the following few hours and patients may find that they pass more urine during this period as this fluid is excreted. Some of this fluid which is blood stained leaks out the small incisions and an absorbent dressing (nappy) is strapped to the shoulder. This is left on overnight and is replaced with small waterproof dressings the next morning so that the patient can shower normally.
This bloody fluid tracks down between the skin layer and muscle and patients may develop quite marked bruising down their arm and over their chest/breast during the week following the operation. This bruising will disappear over 2 -3 weeks.
ANAESTHESIA
This is done with a general anaesthetic and a regional block. It can be done with a block alone but the patient is placed into a seated position on the operating table which can be uncomfortable and thus a general anaesthetic is preferred. The block is done with local anaesthetic injected into the side of the neck where the nerves to the arm are passing. This provides excellent pain relief during the operation thus less anaesthetic drugs are required, patients thus wake up quite refreshed afterwards. The block provides excellent relieve of pain after the operation and lasts for between 8 and 24 hours. The arm may be completely dead and the patient may not even be able to move their fingers initially. Care must be taken not to put anything hot on the arm as this will not be felt and a burn may occur. In approximately 1% of cases there may be a persisting area of numbness in the arm, forearm or hand which usually disappears within 3 months. Occasionally neuralgia (nerve pain) may occur after the block and may require medication till it settles of its own accord.
HOSPITAL STAY
Patients come in on the day of the operation and may be discharged a few hours after the operation or may stay overnight depending on the operation performed and how they are feeling.
MEDICATION
An anti-inflammatory and a pain killer are prescribed. The anti-inflammatory is taken for a week and the pain killer if and when necessary. Most patients take the pain killer for an average of 5 days after the operation. Some patients however don’t take any medication whereas other patients may need pain killers for up to 6 weeks. This is dependent on the individual and the operation performed. More pain is usually felt following a rotator cuff repair. Patients often struggle to sleep initially and a sleeping tablet may be required.
SLEEP
Patients often have difficulty sleeping and besides taking sleeping tablets, sleeping propped up with pillows or sleeping in a chair will be easier. A recliner (lazy boy chair) will often be the best option.
Anaesthesia
The anaesthetist will see you in the ward prior to the operation or in the reception room in theatre. If you have medical problems; eg: heart condition, previous cardiac surgery, chest disease (eg: emphysema), you will be referred to a physician for an assessment and may see the anaesthetist a few days prior to the operation. A premed is sometimes given prior to theatre which will make you a little drowsy and relaxed. In theatre you will sit on the theatre table and make yourself comfortable prior to the induction of anaesthesia. A drip will be inserted into your arm through which the anaesthetic drugs are administered. Gases will be given by a mask and once you are asleep a tube will be inserted into your throat, this is why you may have a sore throat for a short time after the operation.
The anesthetic is a general anaesthetic with a regional block. It can be done with a block alone but you are placed into a seated position on the operating table which can be uncomfortable and thus a general anaesthetic is preferred. The block is done with local anaesthetic injected into the side of the neck where the nerves to the arm are passing (essentially an epidural of the arm). This provides excellent pain relief during the operation thus less anaesthetic drugs are required; you tend to wake up quickly and are quite refreshed afterwards. The block provides excellent relieve of pain after the operation and lasts for between 8 and 24 hours. The arm may be completely dead and you may not even be able to move your fingers initially. Care must be taken not to put anything hot on the arm as this will not be felt and a burn may occur. In approximately 1% of cases there may be a persisting area of numbness in the arm, forearm or hand after the block has worn off. This numbness will usually disappear within 3 months. Occasionally neuralgia (nerve pain) may occur after the block and may require medication till it settles of its own accord. Although extremely rare, permanent nerve damage has been reported.
You tend to wake up very quickly after the operation and may eat soon afterwards. The drip will be taken down when you are back in the ward. The block provides excellent pain relief for between 8 and 24 hours but pain killers and anti-inflammatories are started before the block wears off so that they are already working when the pain starts. Patients vary in the amount of pain killers that they need; some don’t need to take any whereas others may need to take them for up to 6 weeks.

