Shoulder Arthritis
The shoulder joint or glenohumeral joint is a ball and socket joint but unlike the hip, the ball
is held against the socket rather than fitting into it. It thus depends on its surrounding structures and in particular the rotator cuff (a group of muscles and tendons that form a hood over the top of the arm bone or humerus); see shoulder anatomy) to keep it together and to control the stability and finer movements. Arthritis of the shoulder joint is much less common than arthritis in the hip and knee joints.
Would you like to see a doctor?
Learn more
Causes
Arthritis occurs when the layer of cartilage on the bones on either side of the joint wears out or is destroyed. The cartilage is normally approximately 3 mm thick and provides a cushion as the bones move against each other. When looking at an x-ray a space is seen between the bony surfaces (fig 1), this space represents the cartilage (which is not seen on a x-ray) and is seen to be wearing when this space decreases (Fig 2).
There are 2 main types of arthritis; osteoarthritis (wear and tear) and inflammatory arthritis (e.g. rheumatoid arthritis).
OSTEOARTHRITIS
A. Primary – Normal wear and tear with aging (when there is no apparent cause).
B. Secondary
i). Trauma – a previous fracture or dislocation of the shoulder; these may damage the cartilage and lead to rough surfaces moving against each other.
ii). Infection – infection may destroy the cartilage
iii). Inherent deformities of the joint – irregular surfaces lead to abnormal wear to the cartilage.
iv). Tear of the rotator cuff tendons – a massive chronic tear of the rotator cuff leads to the ball riding up and not staying against the socket or glenoid. This leads to abnormal wear as the surfaces are no longer concentric.
INFLAMMATORY
The most common type is rheumatoid arthritis where destruction of the cartilage is due to an autoimmune reaction i.e. bodies own antibodies destroy the cartilage.
Diagnosis
Patients present with increasing pain and decreasing range of movement. The diagnosis is usually easily made from the X-rays.
Treatment
This depends on the severity of the patient’s symptoms. There are patients with advanced arthritis of their shoulders who have little or no pain. Treatment is not necessary in these patients. Some patients have moderate or intermittent pain which may be controlled with occasional or regular non steroidal anti-inflammatory drugs. Cortisone injections into the joint may give periods of relief from the pain.
In younger patients an arthroscopic debridement may be done. This is a relatively minor procedure where a telescope is inserted through key holes and the inflammation and bony spurs are removed from the joint. This is helpful in approximately 70 % of patients and the aim is to delay more extensive surgery in the younger patient. Interpostion arthroplasty where a piece of tissue is inserted between the joint surfaces may be used in the younger patient. The results of this are unpredictable with reports varying on its effectiveness and merits. It may result in improvement in approximately 50% of patients and again is used as a temporizing measure to delay more extensive surgery.
Shoulder Replacement
Major advances have been made with design over the years and it has become a very successful procedure for shoulder arthritis. Unlike the hip it is not always necessary to replace both sides of the joint, though most reports show that replacing both the ball and socket is preferable. It is not always however possible to replace the socket i.e. when the bone of the socket is extremely worn or if the rotator cuff tendons are torn or not functioning.
In the younger patient a resurfacing prosthesis may be used where a cap is fitted over the end of the bone rather than cutting off the head of the humerus (Fig. 3).

In the conventional prosthesis a stem is passed down the centre of the humerus and the appropriate size head applied. The socket is replaced with a plastic component (Fig. 4).
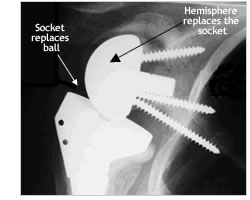
Fig. 5 – Reverse Prosthesis
In complex cases and where there is no functioning rotator cuff, a reverse prosthesis may be used. This has revolutionised the treatment of these cases where the patient has extreme limitation of function as well as pain. In this prosthesis the socket or glenoid is replaced with a hemisphere and the ball or humeral head replaced with a socket (Fig. 5). This unusual prosthesis often restores the function in the patients arm.




